2024 Flu and COVID-19 Vaccine FAQ

Do you have questions about what to expect during this year’s flu season? As your partner in health, we’re answering your commonly asked questions about flu and COVID-19 virulence and how you can best protect yourself and others.
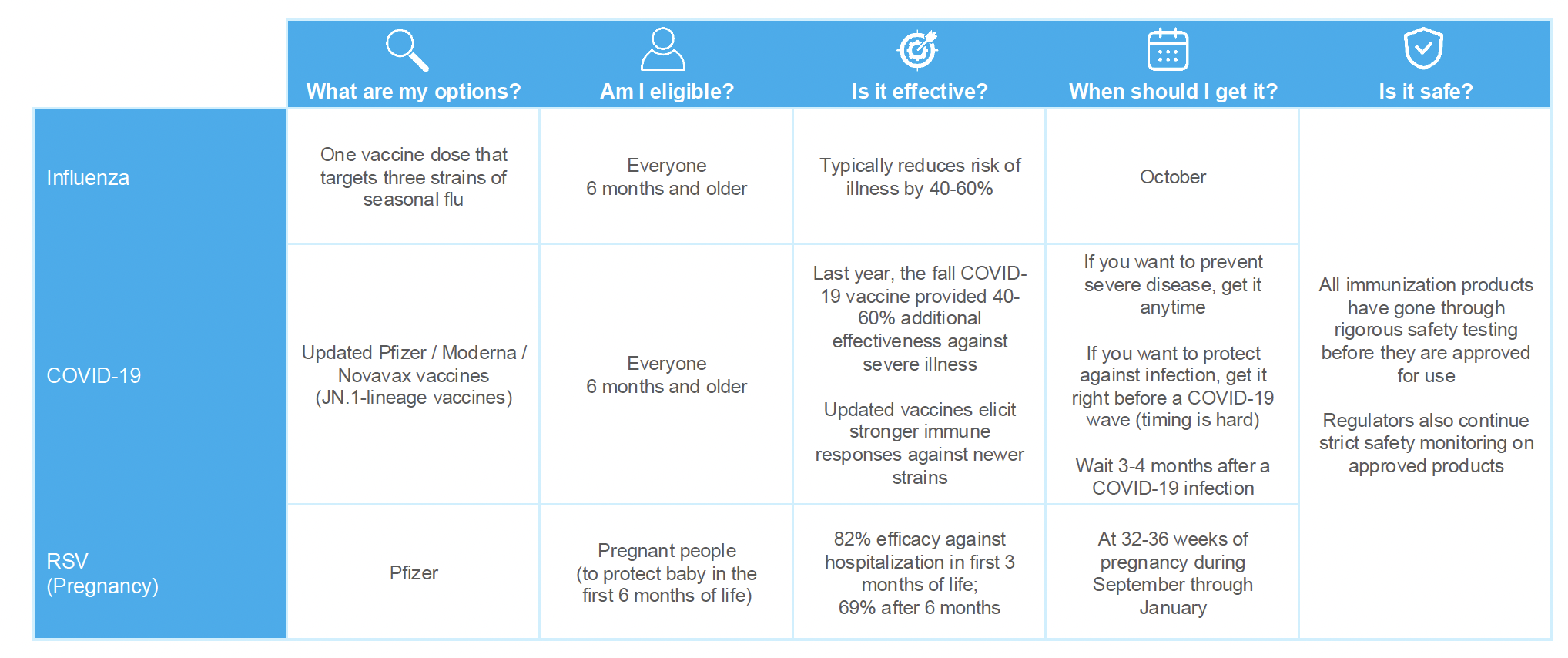
Are the COVID-19 and influenza vaccines safe? What are the side effects?
The FDA and CDC made their recommendations after reviewing the available safety evidence and concluding that the potential benefits of the updated vaccines outweigh any potential harms. You cannot get the actual illness from the COVID-19 and influenza vaccines. Potential mild side effects may include sore arm and a low-grade fever, but these usually go away in 1-2 days. Severe adverse reactions to both vaccines are extremely rare. While some people have developed heart problems after an mRNA COVID-19 vaccination, including myocarditis or pericarditis, the risk is extremely low. There is no risk of developing myocarditis or pericarditis after an influenza vaccine.
Where can I get these vaccines?
Flu vaccines will be available at the Barclays Health Centers this Fall. COVID-19 vaccines should be available at your local pharmacy or doctor’s office. If you are interested in exploring resources for vaccination, we recommend checking availability and finding additional information at vaccines.gov.
When can I get the COVID-19 and influenza vaccines?
The CDC recommends getting these vaccines in September and October to be protected for the fall respiratory season.
Can I get the COVID-19 and influenza vaccines at the same time?
Yes, you can get your COVID-19 and influenza vaccines at the same time. However, you may want to get the shots in different arms. The CDC, other scientists, and regulatory agencies around the world have reviewed the available data and concluded it is safe to do so and does not affect the efficacy of the shots. Some people may want to get them on different days to minimize any temporary side effects, such as soreness, low-grade fever, fatigue.
When can I get the 2024–2025 COVID-19 vaccine, if I had COVID-19 this summer?
If you recently had COVID-19 you should wait 3 months before getting an updated vaccine. Recent infection from COVID-19 provides protection against COVID-19 but protection will decrease over time.
What is the difference between an mRNA (Moderna/ Pfizer) and protein subunit based (Novavax) vaccine?
An mRNA vaccine uses messenger (“m”) RNA created in the lab to teach our own cells to make a spike protein that is found on COVID-19 cells. These spike proteins then trigger our immune response to create antibodies, which provide protection against infection. A protein subunit-based vaccine contains pieces of spike protein found in COVID-19 cells. These spike proteins trigger our immune response to create antibodies. The COVID-19 vaccines do not use any live virus and cannot cause infection of COVID-19.
Which updated COVID-19 vaccine should I get?
We recommend getting whichever vaccine is available. Beyond the difference in age criteria and composition, there are no practical differences in effectiveness or safety between the Pfizer and Moderna mRNA vaccines. While the mRNA vaccines target Omicron KP.2, a slightly more recent strain that started to circulate widely in spring 2024, the JN.1 strain that the Novavax vaccine targets is also a good match to the strains circulating right now because KP.2 has descended from JN.1. If you are currently eligible and have questions about which vaccine you should receive, we recommend speaking to your health care provider for more information.